New results reveal 90 percent patients with transfusion-dependent β-thalassemia no longer required monthly blood transfusions years after receiving gene therapy. The Phase III trial enrolled 22 patients, 20 of which (91 percent), including six of the seven patients (86 percent) who were younger than 12 years of age, achieved transfusion independence.
“It is impressive that so many patients in the study, including the youngest patients, acquired transfusion independence that was durable,” stated study co-author Dr Jennifer Schneiderman, from the Center for Cancer and Blood Disorders at Ann & Robert H. Lurie Children’s Hospital of Chicago and Associate Professor of Pediatrics at Northwestern University Feinberg School of Medicine, both US.
“At Lurie Children’s, we have participated in these gene therapy trials from the earliest stages and have been enrolling patients for close to a decade. The current study represents the next step in moving this intervention into clinical practice, which will increase access to a potential cure for patients with transfusion-dependent thalassemia.”
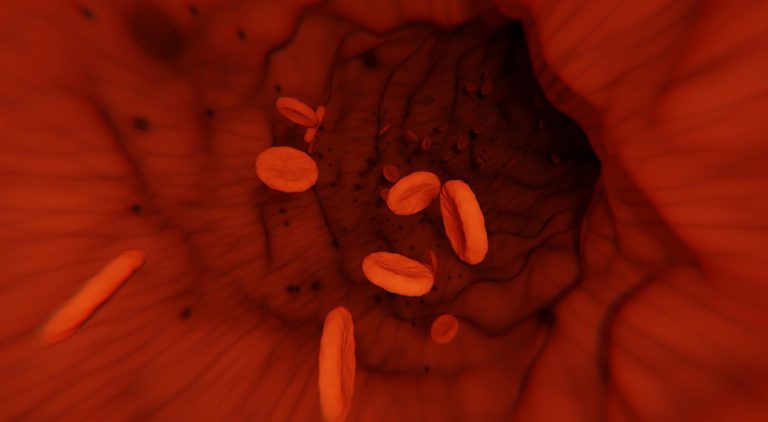
β-thalassemia patients do not produce sufficient functional haemoglobin in their red blood cells, disrupting oxygen transfer within the body. Those with the most severe type of the disease require red blood cell transfusions every month for survival.
Frequent transfusions, however, can cause serious complications due to iron overload and infections, especially if the patient’s spleen has been removed.
Read more: Pakistan reports over 1,400 coronavirus cases,18 deaths
Haematopoietic stem cell transplantation from someone who makes functional haemoglobin can be a potentially curative treatment for β-thalassemia, but it requires a well-matched donor, which can be difficult to find. It also poses a risk for graft versus host disease.
The trial evaluated an ex vivo gene therapy, Betibeglogene autotemcel (beti-cel), containing autologous CD34+ haematopoietic stem cells and progenitor cells transduced with the BB305 lentiviral vector encoding the functional β-globin (βA-T87Q) gene. Before the modified cells are infused to the patients, they are treated with chemotherapy.
Patients typically reached transfusion-free status about one month after the autologous stem cell transplantation. Patients reported in the paper had been monitored for a range of 13 months to four years after receiving their new cells.